Vaccines save millions of lives worldwide annually, offering longer, healthier lives. However, vaccination disparities persist, particularly during the COVID-19 pandemic, with economic, racial, and ethnic gaps affecting adult vaccine uptake. To tackle these challenges, understanding the COVID-19 Vaccine Coverage Index (CVAC) and the impact of vaccine hesitancy on vaccination rates is crucial.
In this blog, we summarize an article we *just* published in Vaccines addressing how the social, structural, and psychological barriers can lead to widespread vaccine coverage.
The COVID-19 Vaccine Coverage Index (CVAC)
The CVAC is a powerful tool designed to uncover barriers to COVID-19 vaccination in vulnerable U.S. counties. It identifies key factors such as sociodemographics, resource-constrained health systems, healthcare accessibility, irregular care-seeking behavior, and historic under-vaccination. Public health professionals and policymakers can develop targeted interventions for better vaccine uptake by analyzing these components.
Understanding Vaccine Hesitancy
Vaccine hesitancy, a behavioral phenomenon, involves delayed or refused vaccinations despite availability. Psychological factors like perceiving lower danger, safety concerns, and conspiracy beliefs contribute to hesitancy. These psychological barriers can be categorized as “3Cs”: complacency, convenience, and confidence. Recognizing vaccine hesitancy is vital in comprehending vaccination trends at a county level.
Approach
We had two research questions:
- Can social and structural barriers, as CVAC measures, predict county-level vaccination rates?
- Does vaccine hesitancy moderate the relationship between social and structural barriers and vaccination rates at the county level?
The study utilizes publicly available county-level data from the U.S. Department of Health and Human Services Household Pulse Survey and the CDC’s county-level COVID-19 Vaccinations in the United States. The measures examined include vaccine coverage, CVAC, vaccine hesitancy, and racial and ethnic characteristics.
We found:
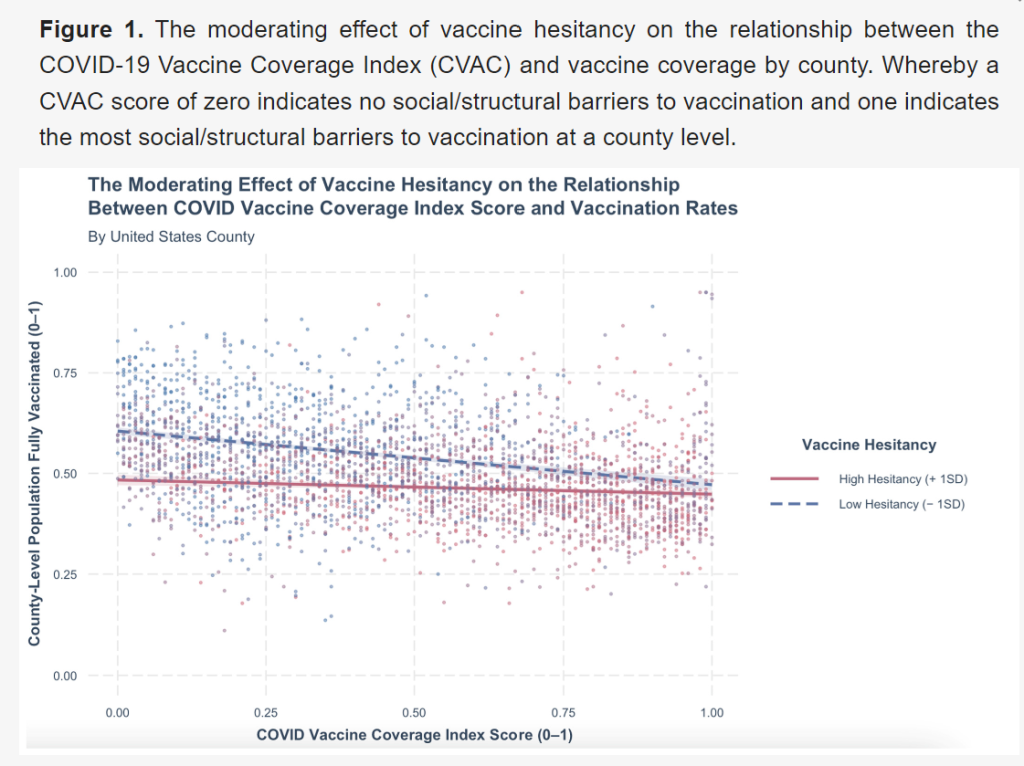
The study reveals that while CVAC moderately predicts county-level vaccine coverage, the model significantly improves when considering vaccine hesitancy. This emphasizes the importance of addressing social and structural barriers alongside psychological factors to increase vaccination rates. Furthermore, vaccine hesitancy significantly influences the relationship between CVAC and vaccine coverage, shedding light on vaccination disparities.
Implications for Health Equity
The study highlights the shared responsibility for vaccination among marginalized populations and socially advantaged groups in achieving herd immunity and promoting health equity. Tailoring interventions to address psychological barriers to vaccination is essential.
Implications for Practice
Public health practitioners should design targeted interventions based on distinct psychological barriers to vaccination among different populations. Understanding vaccine hesitancy personas, such as the enthusiasts, the watchful, the cost-anxious, the system distrusters, and the skeptics, can guide message creation to increase vaccine uptake.
Conclusion
To achieve widespread vaccine coverage and protect communities during pandemics, addressing social, structural, and psychological barriers to vaccination is vital. By developing targeted interventions, we can promote equitable vaccination and ensure a healthier future for all.

